What Everyone Should Know About Atherosclerosis in 2024
Disclaimer: I am not a doctor. This is NOT medical advice. Please talk to your doctor before changing anything in your diet, exercise, lifestyle, or medications.
In 1948 the Framingham Heart Study identified the initial risk factors that are associated with atherosclerosis. We learned the dangers of things like high blood pressure and smoking. Forty years later, in 1988, the US guidelines defined total cholesterol under 200 mg/dL as low risk. A few years later, the guideline changed to focus on LDL-C rather than total cholesterol. Around the same time, we recognized the potential positive value of HDL-C and started watching HDL-C/LDL-C ratios. The current US guidelines, out in 2013, removed these guidelines and moved to a risk assessment model. The goalpost has been moving as we learn more about the disease. It’s good to “get it right” but can be confusing for people trying to manage their risk.
I remember first becoming aware of these changes in the mid-1990’s because I was a high-risk individual (family history) but had “moderate” cholesterol numbers. As I’ve researched to understand my true risks better, I’ve realized that we’ve come a long way in our thinking since then, but we haven’t made these new learnings mainstream. This means your doctor may or may not know about them, and may or may not believe them. My goal is to make you aware of current thinking related to atherosclerosis so that you can have educated conversations with your healthcare provider. I am not a doctor.
First, plaque (aka atherosclerosis) builds up inside our arterial walls. Back in the 1990’s, this was understood but not well communicated. The process is something like this:
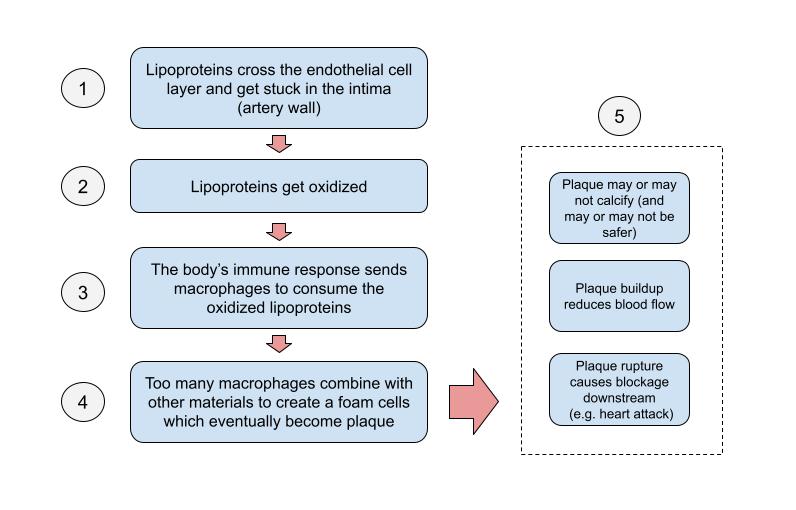
Simplified process of plaque development
Lipoproteins transport cholesterol and triglycerides in your blood. Damage to your artery walls can increase the number of lipoproteins that get through, but it's a natural process. It’s speculated that we might need this permeability as part of our immune system. Lipoproteins that get into our arteries will eventually go away, but if they get oxidized then they can trigger an immune response. This is another natural process. The problem is when too many oxidized particles exist and the immune system kicks into overdrive.
In the end, it's a numbers game, which is why statins are effective. They reduce the number of lipoproteins, which decreases the chance of your immune system going overboard. The problem with statins is that just looking at your lipoproteins provides an incomplete picture of the process. The full picture requires also considering:
- The health of your artery walls: Healthy arteries existing in a healthy environment can reduce the amount of particles that get through. Two major drivers of arterial health are blood pressure and diabetes. High blood pressure doesn’t necessarily damage your arteries (they are very sturdy), but it does make it easier for particles to cross the endothelium. Diabetes means being unable to clear glucose from your blood, and the extra glucose damages artery walls.
- Oxidation levels: If we could prevent oxidation from happening then there would be no immune response, but unfortunately studies to reduce oxidation, such as with Vitamin E supplementation (an anti-oxidant), have had worse overall results.
- Your immune response: Reducing your immune response can prevent the runaway process from starting. Having an immune system is important, so we don’t want to stop it completely. The problem appears to be chronic inflammation. Chronic inflammatory conditions such as gum disease, frozen shoulder, and Crohn’s disease have all been linked to atherosclerosis.
- Hereditary risk: According to Dr. Thomas Dayspring, an expert on the subject, there are also at least two inherited conditions that some people have to manage. The first condition is people that have a high Lp(a) count, which makes lipoproteins more “sticky,” and the second condition is people with unusually high triglyceride levels.
So, what did most doctors do 10 years ago? They order a lipid panel as part of your blood test and then review the cholesterol numbers. This is not bad, but as I’ve just outlined, it’s incomplete. Here’s a more complete picture of what you should be measuring:
- Blood pressure. Luckily, this is part of almost every doctor visit.
- Metabolic Syndrome (i.e. Diabetes). Most physicals include a fasting blood glucose level, but there are more accurate tests now available. One, called HbA1C, actually measures your average blood glucose levels over approximately 3 months. Another, OGTT (Oral Glucose Tolerance Test), is more intensive, but it measures your ability to clear out glucose from your blood.
- Lipoprotein count. We can measure the number of lipoproteins in our blood with a test called ApoB. Each lipoprotein has one ApoB particle, so measuring one gives us both counts. This will be more accurate than measuring cholesterol.
- Inflammation levels. The most popular test for this is hs-CRP. The problem is that, if you are sick, these numbers can be temporarily inflated, but over time they will give a better indication of chronic inflammation levels.
- Triglycerides and Lp(a). Luckily, triglycerides are part of the standard lipid panel. Get your La(a) measured at least once to know if it’s a risk factor for you.
What do I do with this information?
I am not a doctor, so I can’t give medical advice. It probably comes down to your situation. If you are high-risk, then make sure your doctor is ordering all these tests for you. If you don’t know your numbers, you should get a copy of your blood test results and keep track of them over time.
When do I need these tests?
Experts suggest that by age 35 you will know your risk profile. I suggest getting these tests done earlier just to create a baseline. I developed high blood pressure by age 25. Again, talk to your doctor.
But my doctor just wants to put me on a statin!
Each person’s situation is different. I take a statin, but I also get severe muscle cramps and weakness from them. To counteract the side effects, I take a supplement called CoQ10. It can be a pain (literally), but for me, it’s worth it, and the CoQ10 really does help. There are also new drugs that can potentially work for you without the side effects.
Some people have had success with low-carb diets. You are reducing your glucose levels with this type of eating, and there is speculation that these diets are also anti-inflammatory, an additional benefit. Be warned, however, that people have still developed atherosclerosis with this type of diet.
If you have high blood pressure, get it treated. Consider supplementing with beets or beetroot. It supports your nitric oxide production, which is a vasodilator (helps your arteries maintain flexibility).
If you have high inflammation levels consider taking an anti-inflammatory supplement. Glucosamine, turmeric, and fish oil all have potential anti-inflammatory properties, but the science of how they help with atherosclerosis, or not, is still TBD.
How do I know if I have atherosclerosis?
There are several tests you can do, but they are imperfect in their assessment and application.
- Carotid Intima-Media Thickness Test (CIMT): This is an ultrasound of the main artery in your neck. It’s accurate, which is great, but it is only measuring one spot. It highlights your risk of stroke, but not of heart attack.
- Coronary Artery Calcium (CAC) Testing: This measures the amount of calcified plaque in the arteries around your heart. The problem with this is that you can have plaque build-up without calcification, so it gives you some indication of your condition but is incomplete. Also, some experts consider that calcification of plaque is your body healing, so having calcification means you have atherosclerosis but not if your condition is worsening. It can take 5–10 years for plaque to calcify. This means your levels can still be going up even if you are successfully treating the disease.
- CT Angiography (CTA): This is a CT Scan of your arteries. It is accurate but prohibitively expensive for most people. I believe it’s generally reserved for people who already have complications from heart disease.
What do I do with all this information?
I know I’ve thrown a lot of stuff out there. I wrote this because I’m in my 50's and I wish I had known all this when I was 30. I’ve already lost more than one friend in my age bracket due to heart attacks. Maybe, with a holistic approach, as I’ve outlined here, their deaths could have been prevented. Talk to your doctor.
Dave DuBois
December 16, 2023