Setting Your Cholesterol Target
Disclaimer: I am not a doctor. This is NOT medical advice. Please talk to your doctor before changing anything in your diet, exercise, lifestyle, or medications.
How Cholesterol Links to Longevity
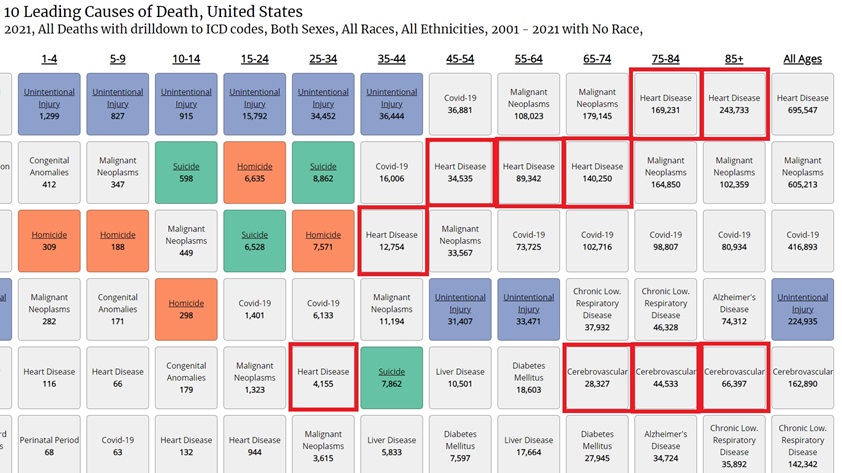
Below is data from the US CDC on the most common causes of death in the US, and I’ve highlighted Heart Disease and Strokes on the list. Unmanaged, the risks from atherosclerosis are real. My mom had a major stroke at age 49, and I’ve had two friends pass away from heart attacks, one in his 40s and one in his 50s. I’m sure everyone has stories like this.
Heart disease becomes the leading cause of death as we age, and the bulk of heart disease stems from atherosclerosis. This is not new information, but the point of this article is to provide data. so here’s data for the US as tracked by the CDC:
Many studies now exist on Centenarians (people who live to 100). The only common link researchers have found is that these people are more resilient. They still suffer from the same ailments as everyone else but are affected later in life. If your goal is living to 100, you must work to prevent atherosclerosis.
Best Way to Measure Cholesterol and other Risk Factors
Research has found that, from the family of lipid measures, ApoB is the best indicator of risk. It indicates how many lipoproteins you have in your blood, the carriers of cholesterol. The analogy is cars and passengers. When we measure cholesterol we are counting passengers, while ApoB is counting cars. They are related, so if you measure one you can approximate the other. Unfortunately, these studies I am referencing use different measures. Sometimes they are looking at Total Cholesterol and sometimes they are looking at LDL-C. This is because ApoB is relatively new and not available in longer-term studies.
Do you have to get your ApoB measured? It depends, if your numbers are great, then probably not, but if they are borderline then it gives you a more accurate picture of your risk. I’ve measured my ApoB 6 times, and my ApoB/non-HDL-C varied from 0.62–0.82, so there is significant variation in these measures (at least for me).
This is not intended as a deep dive into ALL the tests one can/should consider for a complete picture of cardiovascular health. That is a discussion for you and your doctor. I am highlighting some tests so that if you are interested it can help guide you on where to do more research.
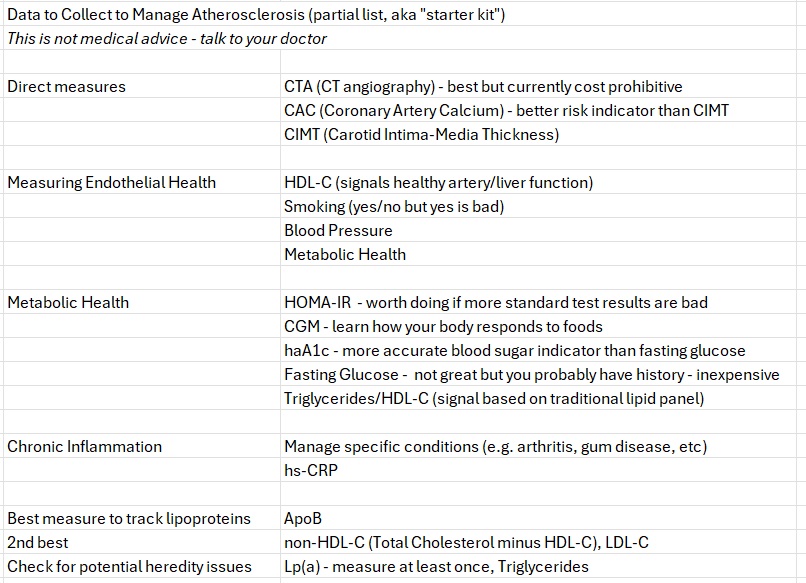
If you are not doing so, you should be saving your test results and tracking over time — don’t just rely on your doctor. You should also consider a baseline CAC test if you are over 40 years old and have not done so — especially if you have known risk factors.
What is a Healthy Cholesterol Level?
In 1985 the Central Automation Laboratory (CALAB) in Stockholm, Sweden started a long-term tracking program called the Swedish AMORIS Cohort. It includes Total Cholesterol (TC) data on centenarians, which I’ve summarized here:
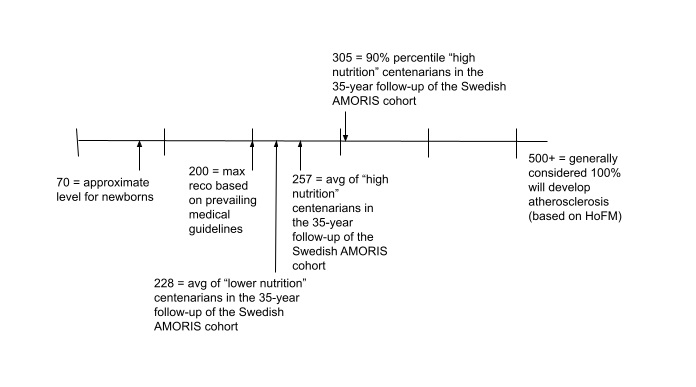
The study used blood work to identify two groups. The group with better overall test results was called the “high nutrition” group, and the other “lower nutrition.” Centenarians, on average, had average TC numbers of 257 and 228 for the two groups, clearly above the maximum recommended TC level of 200.
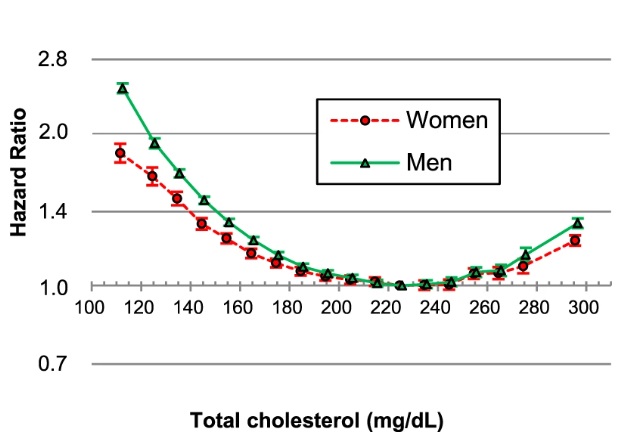
Here is the results from another study that followed 12 million Koreans for 10 years.
You can see from the data that the optimum TC was around 230. Guidelines vary from country to country, but generally most recommendations are for TC below 200 or even lower. What gives?
First, these analyses identify correlation, not causation. This does NOT mean that cholesterol doesn’t matter, or that doctors are lying to us. Instead, it’s fair to say TC ~230 is probably a good number for healthy individuals who do not have any of the conditions that lead to atherosclerosis.
Does this mean the recommendations are wrong? No, because if looking at lipid data in isolation, or can isolate and account for related factors, you will see that data suggests the lower targets are justified.
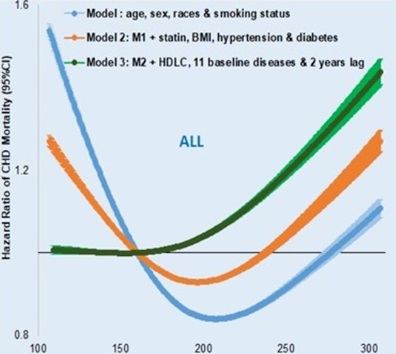
Here is a recent 10-year follow-up study of 4 million veterans.
Interestingly, the first model, which was the least complex, identified the optimum TC at 207 mg/dL. As they accounted for other factors, such as HDL-C and other diseases, they identified the optimum TC<180 mg/dL.
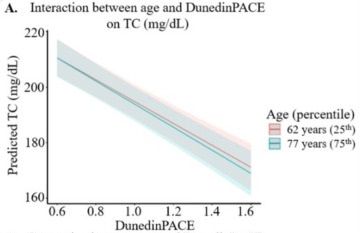
Finally, here is a recent analysis that looked at blood markers that indicate our pace of aging (how our blood tests compare to our actual age). Higher TC, to a degree, is better for aging:
The lower your DunedinPACE value the "slower" you are aging according to your epigenetics.
Relationship Between Cholesterol and Atherosclerosis
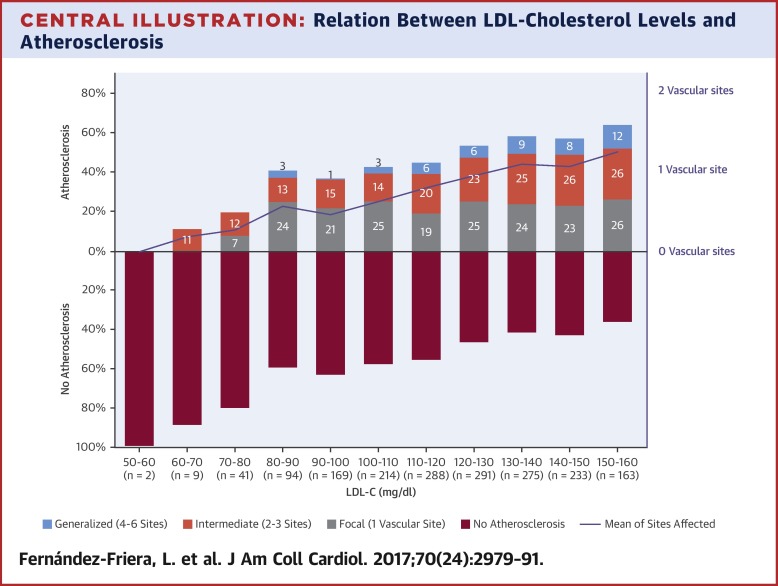
Most cholesterol analyses use LDL-C as it’s been the focus of medical research. This result from a 2017, 4000-person study drives home why our current guidelines exist. Looking at LDL-C in isolation, you need low numbers (e.g. LDL-C < 70) to have a high confidence in preventing atherosclerosis.
Note that the number of participants in each bracket is low, and this is proportional data, so assume a wide confidence interval in this data. The trend is more important than the actual percentages. This also clearly shows that even at high cholesterol levels a portion of the population has no atherosclerosis, so LDL-C CAN NOT be the only factor.
Relationship between Blood Pressure and CHD Incidents
There is no question that high blood pressure is one of the leading contributors to atherosclerosis. Intuitively, this explains why different people generally develop blockages at the same locations in their arteries (higher stress spots) and why we don’t develop atherosclerosis in our veins (lower pressure than arteries).
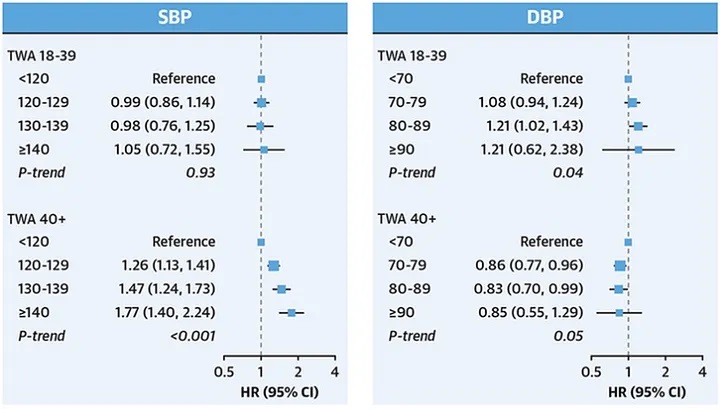
Interestingly, this study of pooled cohort data found that below age 39 (TWA 18–39) diastolic blood pressure was the higher risk factor, but that above age 39 systolic blood pressure was the higher risk.
Overall, reducing your Systolic BP as low as possible, and below 120 if you can, will have the biggest impact on your risk.
Blood pressure is difficult to measure as it’s highly variable. If you are at risk, learn to measure it correctly. Think of it like measuring your car’s RPMs. When you measure blood pressure it’s like trying to measure your car’s RPMs at idle. Anything you do that revs up the engine will make the measure incorrect for comparison purposes.
Also, arteries are strong. They can handle pressures up to 10 times higher than normal blood pressure. We are worried about chronically higher “idle” blood pressure, not short-term increases — unless you have plaque. If you have plaque then higher blood pressure increases the chances of rupture (aka heart attack). It is normal for systolic blood pressure to reach 180–200 during exercise, which is why you need to be careful if you suspect or know you have plaque buildup, and this is why you should check with your doctor before starting new exercise programs.
Relationship between Blood Sugar and Atherosclerosis
We also know that higher blood sugar contributes to blood disease. My understanding is that glucose in our blood binds with particles and these particles damage the walls of our arteries. I’ve not found a lot of writing on the subject, but diabetics are known to suffer from circulation issues and glaucoma, so this tracks.
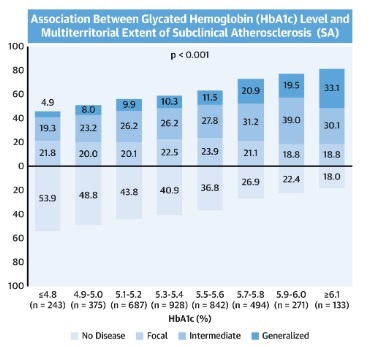
Here is a study that shows the relationship between plaque development and blood sugar, using the hbA1c measure.
What shocked me was the range of values this is reporting. These numbers are all in the “healthy range” of blood sugar (Type 2 Diabetes is hbA1c > 6.5). It looks like your risk of atherosclerosis doubles as your hbA1c goes from 5 to 6, so even if you are not diabetic you should be working to improve your metabolic health. You want to reduce your simple carbohydrate intake (aka sugar) and have a healthy insulin response for when you do indulge.
I’ve moved to artificial sweeteners to help manage my blood sugar. They do seem to help. Studies have associated artificial sweeteners with an additional risk of atherosclerosis, but the risks are much lower, and again, correlation is not causation. We need more data in this area, but for now, they appear to be a good alternative to sugar to help with atherosclerosis.
Inflammation
Almost every chronic inflammatory disease can be associated with atherosclerosis. If you can’t eliminate these diseases, then you want to manage them as best as you can. For instance, I suffer from arthritis, gout, and I have a frozen shoulder. These are all inflammatory conditions. I am countering these with exercise, glucosamine & chondroitin, fish oil, and a low-dose statin. Is it working? It’s hard to say, but I believe so. Talk to your doctor.
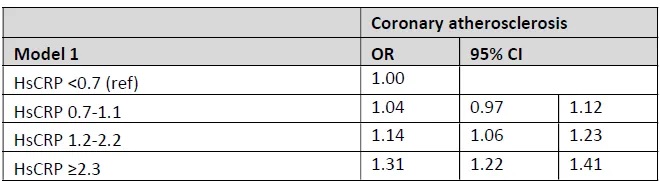
Here is a Swedish study of 25,408 where they were able to look at CTA scans and directly measure atherosclerosis vs inflammation (hs-CRP).
You can see that higher inflammation levels increase risk (when using hazards OR stands for odds ratio). In the same study, however, the authors did not see additional value in adding hs-CRP to standard treatment plans. Why? Because the data suggested that a person’s BMI was as accurate as hs-CRP when evaluating risk due to inflammation.
Should you measure hs-CRP? It depends on your risk profile. I’ve measured mine 3 times now, so I have a baseline. If I have a major change in my diet or health I would measure again to see the impact.
What about Oxidation?
Cardiovascular oxidation is part of the atherosclerosis process. In theory, if we reduce oxidation we will reduce risk. Unfortunately, I have not found studies yet to support this. There are anecdotal references to diet, specifically reducing Omega-6 fats, as reducing oxidation, but nothing evidence-based. In addition, studies promoting supplementation with anti-oxidants have shown the reverse effect, increasing the risk of mortality. Oxidation at some levels is healthy.
Measuring Atherosclerosis
In a perfect world, we could measure each person’s level of atherosclerosis and use it as part of our treatment plan. The problem is that the only way to do this is with a coronary CT angiography, which is prohibitively expensive.
The next closest things are two tests, the Cartoid Intima-Media Thickness (CIMT) test, and the Coronary Artery Calcium (CAC) test. The CIMT measures blood flow in your neck (stroke risk) and the CAC measures calcium buildup in the arteries around your heart (heart attack risk). Of the two, studies indicate that the CAC test is the better predictor of risk, but it has many issues with how to interpret the results.
Calcification of plaque is considered the last stage of the atherosclerotic process. Some experts refer to it as the healing process. Calcified plaque is stable and does not rupture and cause heart attacks. It also takes 5–10 years to develop. This means, at best, it is a lagging indicator. Using myself as an example, I had a CIMT done, which showed no atherosclerosis in my neck, and a CAC test which showed small amounts of calcified plaque in two arteries. How do I interpret this? It validates I need to manage my atherosclerosis, but I already knew that because of my family history. My optimistic interpretation: I was starting to develop plaque but the treatment plan I outlined above is working to prevent further buildup.
Going forward, I will use the CAC test to measure my disease progression. I am 54 years old, so I will get the test done every 3–5 years so that by age 65 I will have multiple data points and an idea of how my treatment plan is working. I started treating my atherosclerosis in 2010, and have continued to add diet and lifestyle changes up to today. Remember, CAC tests do not show soft plaque, so you CAN NOT assume a 0 score means you can ignore the disease. Even if my CAC score remains the same I could still be developing soft plaque.
Summary
There is growing evidence that lower cholesterol is not always beneficial for longevity. This does NOT mean you should ignore it. Instead, make sure you are managing the conditions that promote atherosclerosis. Once you have a handle on your endothelial health and are managing your chronic inflammation, consider direct tests to help understand your risk and disease progression (knowing they are imperfect). Finally, work with your doctor to factor all these elements into a cholesterol (ideally ApoB) target that compliments your holistic treatment plan.
Dave DuBois
April 5, 2024